Margo Girardi, MD, SFHM, and Gina LaRossa, MD, contributed to an abstract and article that were featured in the Society of Hospital Medicine’s Journal of Hospital Medicine. The article, titled “Putting SQuID on the menu: A subcutaneous insulin protocol for diabetic ketoacidosis,” demonstrates how using a subcutaneous insulin protocol on hospitalist units for low-to-moderate severity DKA reduces ICU admissions and ED length of stay.
“We aimed to implement the SQuID protocol on inpatient hospitalist units to decrease ICU admissions, maintain safe patient outcomes, and enhance clinician satisfaction, thus addressing critical aspects of hospital efficiency and patient care.”
The project began in 2021, when several physicians from the WashU School of Medicine identified a problem with limited ICU beds and emergency department overcrowding. “The treatment of DKA is well established but complex, including treatment with intravenous (IV) insulin and frequent monitoring,” the article explained. In cases of low to moderate severity DKA, patients are most often managed in the ED until DKA is resolved and IV insulin is discontinued due to limited ICU resources, resulting in prolonged length of stay and ED crowding. Initially, the SQuID protocol was instituted on a hospitalist-run-12-bed inpatient observation unit. From March 2023 to March 2024, a subsequent project was initiated expanding admissions to a single, 22-bed floor for complex non-ICU medicine patients at Barnes-Jewish Hospital.
Prior to expansion, it was imperative to educate the ED and floor nursing staff, as well as ED and Hospital Medicine physicians to ensure the project’s success. Electronic communications, unit-displayed handouts, and in-person communication sessions were some of the methods used to assist with SQuID protocol implementation. Additionally, best practice advisories (BPAs) and order sets in Epic EMR helped to ensure timely and easy implementation for nurses and physicians alike.
Project Results
Over a 12-month period of 84 patients with LTM DKA, 62 (74%) were treated with SQuID and 22 with IV insulin (Table 1).
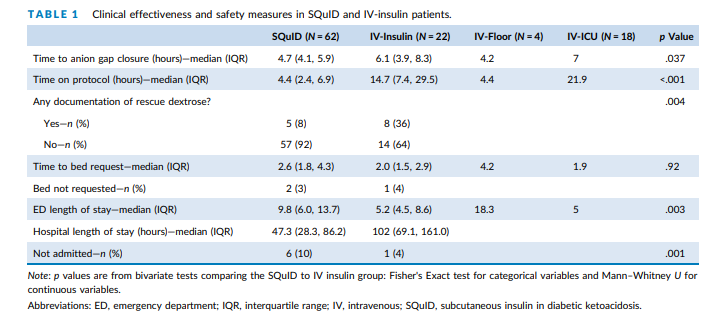
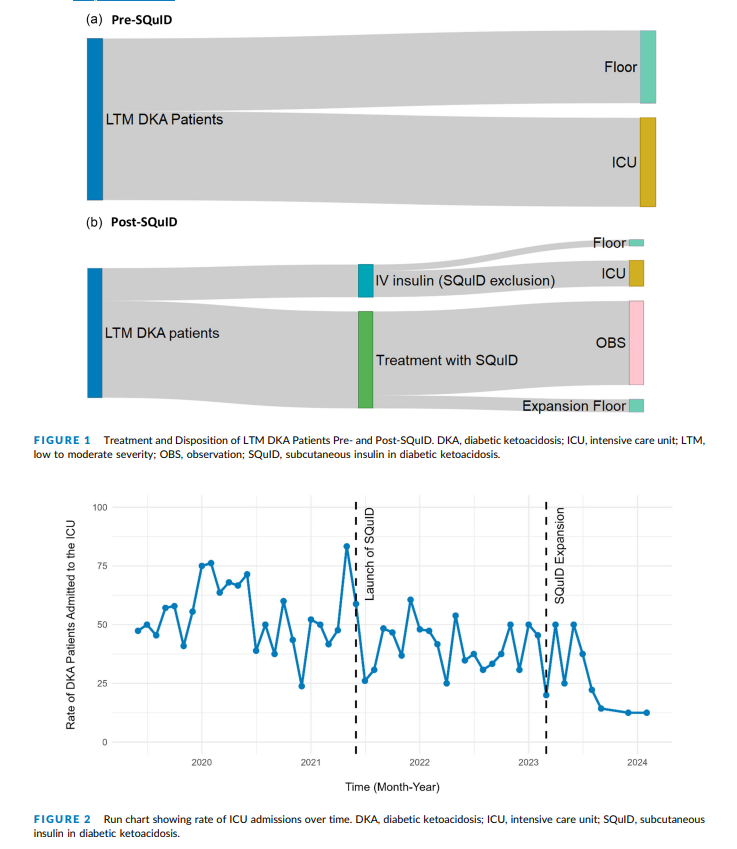
“Essentially all LTM DKA patients without an exclusion criterion are now treated on the SQuID protocol in a non-ICU setting under the care of Hospital Medicine attendings. Since the launch of our protocol, we have reduced ICU admissions for LTM DKA by over 33%.”
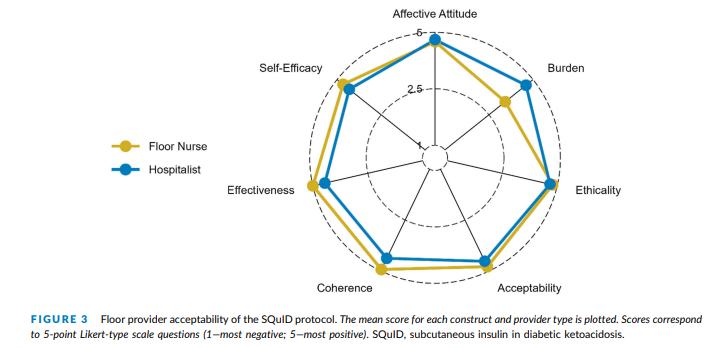
Clinician acceptability was high, with over 90% reporting a favorable experience with the protocols based on survey data (Figure 3).
Key Lessons
The project initially began with the lowest severity patients. As clinicians grew more comfortable and familiar with the protocol, it was expanded to include all low to moderate cases of DKA using SQ insulin, provided that patients did not require ICU admission for reasons other than DKA or have any other exclusion criteria. Throughout the project, several key factors for success and potential pitfalls were identified.
- Nursing-driven protocol: A simple protocol that reduces the workload for hospitalist physicians led to safe and effective treatment with high approval from clinicians.
- Enhanced patient flow and reduced handoffs: Earlier admissions to the floor and reduced handoffs between physicians and nurses improve diabetes education and enhance discharge planning for patients.
- Delays in administering glargine risks rebounding DKA: A major risk to be aware of is the potential resurgence of DKA if there is a delay in administering glargine. It is crucial to educate staff and consider implementing a BPA alert to ensure timely administration to patients.
- Hypoglycemia prevention through timely dextrose administration: Although overall safety was maintained, all observed cases of hypoglycemia requiring rescue dextrose were due to delays in administering dextrose-containing fluids according to protocol (when glucose <250). To prevent this issue, staff education and the implementation of a BPA alert for timely administration are important.
Acknowledgements
Special thanks to the clinicians from the WashU Departments of Internal Medicine and Emergency Medicine, and WashU Divisions of Hospital Medicine and Endocrinology involved in this project:
Margo Girardo, MD, SFHM, Richard T. Griffey, MD, MPH, Ryan M. Schneider, MSN, ACNP-BC, CPPS, Gina LaRossa, MD, Julianne Yeary PharmD, BCCCP, Taylor Kaiser, MPH, Rachel Ancona, PhD, Dan Suarez, MD, and Paulina Cruz-Bravo, MD.
The authors did receive support funding through a Foundation for Barnes‐Jewish Hospital Grant.
Girardi M, Griffey RT, Schneider RM,
et al. Putting SQuID on the menu: a subcutaneous insulin
protocol for diabetic ketoacidosis. J Hosp Med. 2025;1‐6.
doi:10.1002/jhm.70140