On Thursday, November 20, 2025, Chief of the Divisions of General Medicine, Geriatrics and Hospital Medicine, Dr. Molly McNairy, conducted a keynote address in the Connor Auditorium of the Farrell Learning and Teaching Center. When Molly McNairy, MD, MSc, joined WashU Medicine, she took on the unique challenge of re-imaging the structure of general medicine, geriatrics, and hospital medicine. Her keynote explored the future of general internal medicine, and how this collaboration between divisions will bring patient care to the next level.
Dr. McNairy was born and raised in Kinston, North Carolina, where she experienced firsthand the impact of the 23% poverty rate in her community. This focus on social justice inspired her to get involved in internal medicine, stemming from her belief that all people deserve equal rights, opportunities, and treatment, regardless of the community or family they were born into. She pursued her undergraduate training at the University of North Carolina at Chapel Hill and went on to receive her M.D. from Harvard Medical School in Boston, Massachusetts. Additionally, she earned a Master of Science degree from the London School of Economics and the London School of Hygiene and Tropical Medicine. She completed her internship and internal medicine residency at Brigham and Women’s Hospital in Boston, followed by a Global Health Equity Fellowship at Brigham and Women’s Hospital.

“Actionable research can fast-track improvements in population health as a powerful voice to the voiceless that addresses the needs and builds the capacity of communities we serve.“
Her early faculty career was focused on working as an academic hospitalist as well as a global health physician with Partners in Health to implement HIV and primary care programs in sub-Saharan Africa. Dr. McNairy realized her passion for research, seeing that it was a tool to change lives- but it must be actionable. “Actionable research can fast-track improvements in population health as a powerful voice to the voiceless that addresses the needs and builds the capacity of communities we serve,” Molly explained. Over the next decade, her work stayed in HIV and also expanded to work on HIV-CVD co-infection and CVD in low-income countries.
It became clear to Dr. McNairy that there were several areas that were important to invest in to facilitate proactive research, faculty development, and improvements in patient care: clinical capacity, health systems, research mentorship, and students. During her time with Weill Cornell Hospital, Molly helped develop the Cornell General Internal Medicine Research Fellowship, which provided research training pathways for academic general internal medicine. Shortly after, she was asked to serve as Chief of Hospital Medicine- within General Internal Medicine at Weill Cornell. She served a group of about 100 faculty members across two hospitals. Dr. McNairy facilitated the growth of their Hospital Medicine program, assisting with improving stakeholder engagement, implementing team leadership, improving clinical operations, and creating clinical and faculty development programs.
Both then and now, Dr. McNairy’s vision remains the same: leverage all the strengths of academic GIM to radically improve health systems and outcomes. But what is academic General Internal Medicine? Well, it began in the 1970s as nationally there was a shift from hospital care to ambulatory medicine, from acute care management to chronic care, and the introduction of prevention in addition to treatment. In academic medical centers, this expanded the need for medical education, which led to the increasing recognition of academic clinical evaluation sciences and clinical epidemiology from an ambulatory setting. As the Division of General Internal Medicine grew, it continued to expand to different medical schools, with over 150 U.S. medical schools having Divisions of GIM by 2010.



This powerful care model helped to develop a collective force of providers who have a strong sense of shared values around the key domains of clinical care, health systems, advocacy and community, medical education, innovation, and research. With internal medicine experts from different fields collaborating, patients can more easily navigate care systems, leading to better health outcomes and longitudinal relationships.
Developed in 1996, Hospital Medicine is one of the fastest growing and largest specialties in internal medicine. By 2018, 71% of newly certified general internists practiced as hospitalists compared with only 8% practicing as outpatient-only physicians. The specialty rapidly developed, with over 62,000 hospitalists by 2024, from just 1,000 in 2000. This field is now substantially larger than any subspecialty of internal medicine, and providers going into GIM-Hospital Medicine are far outpacing other groups, particularly primary care.
GIM Hospitalists demonstrate expertise in a variety of areas, such as education and research. Studies show that where access to primary care is higher, patients have lower death rates from cancer, heart disease, and strokes, also reducing emergency room visits, hospitalizations, and surgeries. As a nation, we would save $67 billion every year if everyone used a primary care provider as their usual source of care, and every additional primary care patient equates to $1 million in downstream revenue (Macinko, Intl J Health Services Research 2007. Starfield et al, Milbank Quarterly 2005. Spann et al, Annuals of Family Medicine 2004). Yet, of the $4.9 trillion currently spent on US healthcare, only 5% is in primary care.
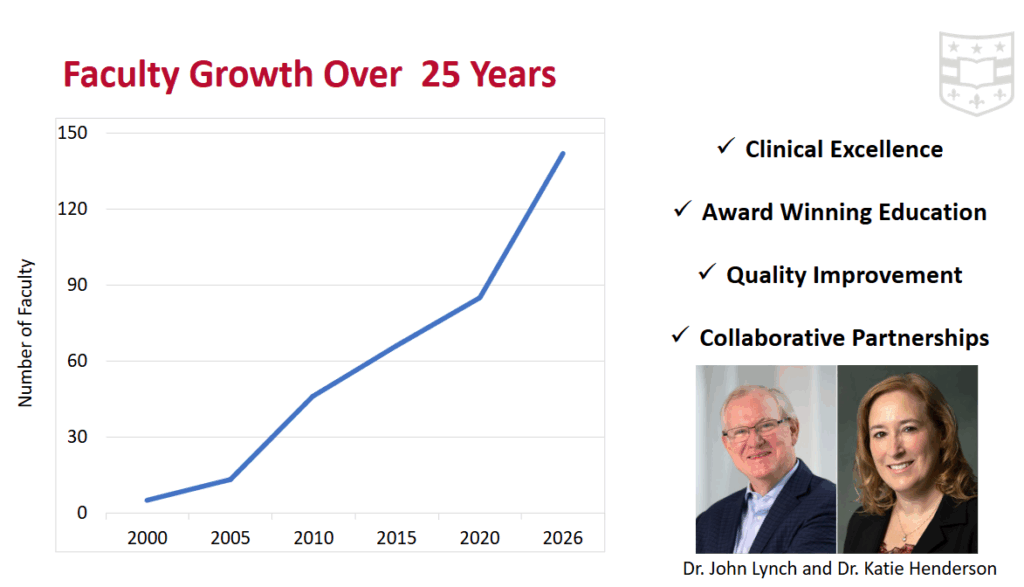
The WashU Division of Hospital Medicine began with just 5 physicians in 2000 and facilitated incredible faculty growth over the last 25 years. WashU hospitalists demonstrate clinical excellence, award-winning education, quality improvement, and collaborative partnerships throughout the hospital. Hospital Medicine has expanded to a variety of clinical service lines and played a key role in leading the hospital through the COVID pandemic in 2020 and beyond. Today, hospital medicine has 142 faculty members, 20 advanced practice providers, and 30 faculty members with over 10 years of experience.
$57.5 million
in clinical billing from FY25
440 patients
per day
13 service lines
across four locations
In 2025, hospitalists were responsible for $57.5 million in clinical billing and managed 19,204 shifts annually, caring for 440 patients daily. They operate across four clinical locations and contribute to 13 different service lines. WashU Hospital Medicine is houses many campus and system leaders, some of whom serve multiple roles across Barnes Jewish Hospital and WashU Medicine.
| Barnes Jewish Hospital | WashU Hospital Medicine |
| Associate Chief Medical Officer: Rachel Bardowell, MD Medical Director of Patient Experience: Patricia Litkowski, MD Unit Medical Directors: Safa Farrag, MD, Margo Girardi, MD Zach Morgan, MD Radha Devi, MD Lead Utilization Management Physician Advisor: Robert Mahoney, MD | Leadership Transition Team: Rachel Bardowell, MD Katy Filson, MD Patricia Litkowski, MD Zach Morgan, MD Section Chief: Michael Lin, MD |
The Division of General Medicine and Geriatrics is committed to advancing individual and community health through exceptional and equitable care, innovative education, and collaborative research. With faculty increasing three times in the past five years, 44 faculty members, and six APPs, GMG is constantly on the uphill in terms of general internal medicine and geriatric care. When it comes to medical education, the GMG Division sees over 454 student and resident rotations annually, scholarship and innovation, Geriatric fellowship, and Education Leadership positions held by GMG faculty members.
In 2025, General Medicine and Geriatrics were responsible for $17.3 million in clinical billing. Our clinic sites at Center for Advanced Medicine (CAM), West County, PCMC Residency Clinic, and our Geriatric sites at BJH, BJWCH, and VA allow us to continue to provide top-notch patient care to our 12,000 patients.
$10.2 million
GMG faculty are PI/Site-PI on 36 grants totaling
$63.6 million
GMG faculty were co-investigators on 40 grants totaling
>140 papers
published by GMG faculty in 2024-2025
In collaboration with our exceptional patient care and education comes our research. Our Research Unit consists of 27 faculty and 47 staff members whose research ranges from clinical epidemiology, health systems, global health, medical decision making, bioethics, and more. In 2025, our research team was PI/Site-PI on 36 grants totaling $10.6 million, were co-investigators on 40 grants totaling at $63.6 million, and authored/co-authored over 140 papers from 2024-2025. On October 29-31, QuEST co-organized the Science for Health Systems Conference that consisted of more than 300 in-person attendees, more than 100 online attendees, and researchers and implementers representing 32 countries across five continents to share health system research methods and findings to maximize health impact.
Education Leadership





Hospital Medicine, General Medicine and Geriatrics, and General Medicine Research are fortunate to have administrative leadership and staff that support the mission as well. Rob Andersson and Rachel Noon serve as Business Directors for Hospital Medicine and General Medicine and Geriatrics – Clinical Unit respectively, and Richard Fair serves as Business Director for the Research Unit of the Division of General Medicine and Geriatrics.
We acknowledge the hard work and dedication that led us here and look forward to the exciting changes that the future brings.
With the divisions that will be merging, there are so many incredible opportunities for synergies, further growth, and greater impact. Collaboration on clinical care, medical education, faculty development, and scholarship/research will allow for even stronger programs that help us to define the culture of internal medicine. As we usher in this new era of WashU General Medicine, each faculty and staff member will play a vital role in building our future by listening and learning from one another, fostering team leadership, creating impactful and strategic plans and community partnerships, expanding clinical research, and growing to last.